Principles of Developmental Primary Care
Principles of Developmental Primary Care
What is Developmental Primary Care?
- The goal of health care is to maximize wellness and function
- We all have things we are good at and things we are not good at
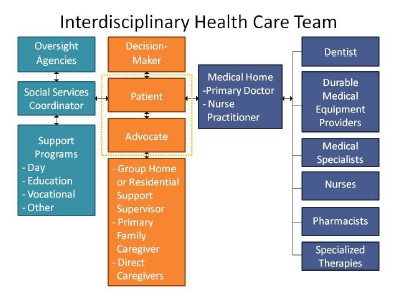
- Health care for people with developmental disabilities is interdisciplinary team-based care with patients and caregivers at the center of the team
- Illness presents as a change in behavior or function
- Everybody communicates, and communication is the foundation of patient care
Guiding Principles
- The lives of people with disabilities are meaningful and valuable
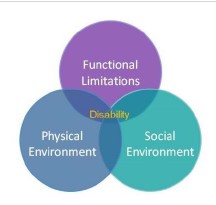
- Reducing disability can be achieved by improving function and/or the social or physical environment
- People have a right to self determination – Nothing About Us Without Us
- Disability is not a characteristic or trait, but a failure to accommodate needs
- Access to care is a civil right
- Inclusion requires action
Neurodiversity
Ability bias is the assumption that able-bodied people are the norm in society, and that people who have disabilities must either strive to become that norm or should keep their distance from abled people. A disability is thus, inherently a “bad” thing that must be overcome. This is often reflected in low expectations, and through the use of dehumanizing language, such as “burden”, “devastating”, “tragic”, “unfortunate”, “suffering”, and “epidemic.”
However, disability is a simple consequence of the human condition. Neurodiversity is the recognition that all people experience the world differently, based on their unique neurological make-up. All experiences are equally valid. Society benefits from different perspectives. The full spectrum of human diversity should be celebrated. 1
The Interdisciplinary Health Care Team
An interdisciplinary health care team is made up of patients and their supporters, health care professionals, and service providers. It includes three categories: the service and support team; the direct care team; and the medical team. Patients and caregivers are at the center of the team. Identifying the role and function of each member is essential to providing quality care. Mapping out the team is the first step to taking a history for a new patient.
Three assessments should be done: caregiver needs, support needs, and accommodations needed for the patient to access care. The needs of caregivers are important and should be considered separately from the patient’s needs. Some patients need additional services and supports in order to partner effectively with their health team. Also, patients may need access to health professionals with specific expertise or to special health services.
The Neurodevelopmental Profile 2
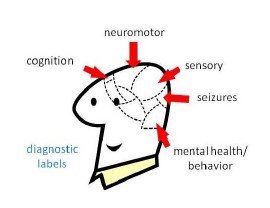
Illness presents as a change in behavior or function. Therefore, it is critical to describe a patient’s baseline traits and characteristics. A neurodevelopmental profile is a summary of an individual’s cognition, neuromotor function, sensory profile, seizure threshold, and mental health/behavior.
A neurodevelopmental profile is a tool to identify both strengths and challenges. Including strengths discourages fixating solely on weaknesses and deficits. Also, comparing current function to the profile helps identify signs of illness which can be overlooked if they are assumed to be a part of a person’s baseline. Some characteristics are associated with specific health risks, such as gum disease and pressure sores. A neurodevelopmental profile is useful to identify risks for preventable complications.
References
- Definition adapted from About.com.
- Adapted from The Five Essential Concepts, American Academy of Developmental Medicine and Dentistry. Available at: www.aadmd.org. Special thanks to Phil May, MD.